How to Change and Clean Your Child's Tracheostomy
A tracheostomy requires regular care to keep the area clean and to prevent infection and skin breakdown. Clean and check skin at least once a day. Some healthcare providers will advise cleanings at least twice a day. Change the tracheostomy (trach) tube as often as you have been told by your healthcare provider. Have two adults present when changing the trach tube, if possible. Follow the general guidelines below and any other specific instructions you are given by your healthcare provider.
Collect supplies
Some people find it helpful to set up and do changing and cleaning in the same place each time. Choose a clean, well-lit space near a sink. Supplies you will need for cleaning and changing include:
-
Rolled-up towel or pillow
-
Liquid soap, alcohol, or disinfectant foam
-
Clean, disposable, powder-less gloves
-
Gauze
-
Normal saline solution
-
Trach ties and scissors, cut to the right length
-
Trach tube
-
Two sterile or disposable cups
-
Small towel
-
Suction machine with catheters
Clean and check the skin
Ask your healthcare provider if your child needs a tracheostomy dressing. If so, change this gauze when cleaning the trach site. Don't use cotton gauze because your child may inhale the tiny fibers. Use only precut gauze. Cutting gauze on your own will cause frayed edges. They increase the risk for infection.
-
Have your child lie on their back in a comfortable position. Put a rolled-up towel under the shoulders.
-
Wash your hands and put on disposable gloves.
-
Clean the neck plate and the skin under it. Use clean gauze pads or other nonfraying material dabbed in normal saline solution.
-
A thorough cleaning technique you may consider involves cleaning the stoma in a stepwise fashion, one quarter at a time. Start at the 12 o'clock position wiping to the 3 o'clock position. Then with a new gauze pad for each section, clean from 12 o'clock to 9 o'clock, followed by the 3 o'clock to 6 o'clock position. Last, clean from the 9 o'clock to 6 o'clock position.
-
Pat the area dry with clean gauze.
-
Check the skin for signs of infection, such as redness, swelling, or warmth.
-
Wash your hands when you finish.
Replace the trach tube
Ask the healthcare provider if you should use an obturator. This device may make it easier to insert the tube. Its rounded edges also protect the stoma during insertion. If you need to use a lubricant, be sure to ask the healthcare provider how much to use. Have a suction machine ready, if needed. Depending on the age of your child, explain the procedure as well as you can to them. If two people are available, one person removes the old trach tube and the other puts the new one in place.
-
Have your child lie on their back in a comfortable position. Put a rolled-up towel under the shoulders.
-
Wash your hands with liquid soap and clean, running water. Dry well. You may also use alcohol or disinfectant foam.
-
Put on disposable gloves.
-
Get the new trach ties ready by draping them around your child’s neck.
-
Open the trach tube package and insert the obturator, if you’re using one, into the new trach tube.
-
Remove the entire old trach tube and lay it down on the towel. Remove gauze if you have used it.
-
Replace the old trach tube right away with the new one. While holding the edges of the tube, remove the obturator right away, if you’re using one. Your child can't breathe if it's left in place.
-
Secure the trach ties.
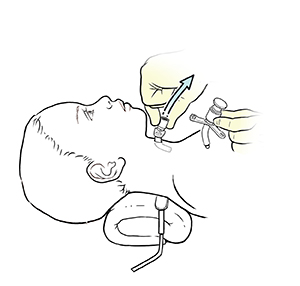 |
| Removing the old trach tube. |
 |
| Inserting the clean trach tube. |
Take precautions with skin care
Unless the area is infected, don't use a hydrogen peroxide mixture directly on the skin. It causes inflammation and increases infection risk. It can also cause mucosal irritation and increase tracheal secretions. Be sure to ask your child's healthcare provider when and if a hydrogen peroxide mixture is OK to use before using it. If a hydrogen peroxide mixture is used on an infected site, it's important to rinse the area with normal saline solution afterward.
Be sure not to get soap or water into the stoma or trach tube. Watch for signs of infection. These include swelling, heat, redness, smelly discharge, fever, or pain when suctioning. If you suspect that the tracheostomy is infected, call your child’s healthcare provider right away.
When to call your child's healthcare provider
Call your child's healthcare provider right away if your child has any of the following:
-
Red or painful stoma
-
Yellow or green, smelly, bloody, or thick mucus from the stoma
-
Fever (see Fever and children, below)
-
Pain when you suction the trach tube
-
Vomiting
-
Trach tube or suction catheter that is hard to insert
Call 911
Call 911 if any of the following occurs:
-
Shortness of breath or any trouble breathing
-
Swelling around the trach tube
-
Large amount of bleeding, or persistent bleeding, from the trach tube
-
Coughing up blood
-
Your child has had a seizure caused by a fever
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider