Total Cystectomy with Continent Urinary Diversion in Women
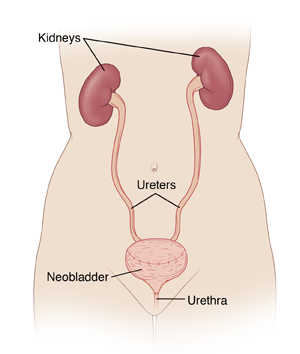
Total cystectomy is surgery to remove the bladder. It is most often done to treat bladder cancer. After the bladder is removed, a new bladder (neobladder) or an internal pouch is made to collect urine. This is called a continent urinary diversion.

Changes to your body
During a simple cystectomy, the bladder is removed. During a radical cystectomy, nearby lymph nodes and organs that the cancer may spread to are also removed. This includes some or all of your reproductive organs, such as the uterus. Removal of these organs means you can no longer become pregnant. If the ovaries are removed, the level of estrogen in your body will drop. This causes your body to go into menopause. Your healthcare provider can tell you more about this and your options.
Types of urinary diversion
To collect urine inside your body, you may have a neobladder or a pouch. Your healthcare provider will discuss which option is best for you.
-
Neobladder. A neobladder allows urine to follow the normal path out of the body. With a neobladder, you’ll no longer have nerves that signal when your bladder is full. You will need to empty the bladder on a set schedule. To do this, you use your pelvic and belly (abdominal) muscles to help push the urine out of your body. In some cases, you pass a thin tube (catheter) through the urethra into the new bladder to drain urine.
-
Pouch. A pouch connects on one end to the tubes (called ureters) that bring urine from the kidneys to the bladder. The other end of the pouch connects to a small, permanent opening (stoma) made in the wall of the belly. Most of the time, the stoma is covered with a small bandage. To empty urine from the pouch, you pass a catheter through the stoma into the pouch. This is done on a set schedule. Unlike some treatments, no bag is needed to collect urine.
-
Urostomy. This is a type of incontinent urinary diversion. The urine flows continually into an external bag through the stoma. This is discussed in a different information sheet.
Getting ready for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your healthcare provider about all medicines you take. This includes prescription medicines and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may be told to stop taking some or all of them before surgery.
-
Follow any directions you are given for not eating or drinking before surgery. If you have been instructed to take medicines, take them with a small sip of water.
-
If you have been told to, prepare your bowel for surgery (called bowel prep). This process begins 1 to 2 days before the surgery. Your provider may tell you to limit your diet to clear liquids. You may also be asked to take laxatives or to give yourself an enema. Follow all instructions you are given.
The day of surgery
The surgery takes 4 to 6 hours. Afterward, you will stay in the hospital for 5 to 7 nights.
Before the surgery begins:
-
An IV (intravenous) line is put into a vein in your arm or hand. This delivers fluids and medicines (such as antibiotics). In some cases, a central or arterial line is put into a vein somewhere else on the body. Your healthcare provider can tell you more.
-
You may be given medicine to prevent blood clots.
-
To keep you pain-free during the surgery, you’re given general anesthesia. This medicine allows you to sleep through the surgery. A tube may be put into your throat to help you breathe.
-
You may have an epidural to help control post-surgery pain. A small tube is put into your back to deliver pain medicine that numbs the lower body. Talk with your provider, anesthesiologist, or nurse anesthetist about this option.
During the surgery:
-
A cut (incision) is made in the lower belly.
-
The lymph nodes near the bladder may be removed. These are checked for cancer cells (a sign that cancer has spread).
-
The bladder is removed. If your surgery is a radical cystectomy, then the nearby reproductive organs are also removed. These include the fallopian tubes, uterus, cervix, and part of the vagina. The ovaries will also likely be removed.
-
For a neobladder, a piece of the small intestine is removed. It is attached to the ureters on one end and to the urethra on the other end.
-
For a pouch, the end of the small intestine and first part of the large intestine is removed. A stoma is made in the wall of your lower belly. The piece of intestine is then connected to the ureters on one end and to the stoma on the other.
-
Thin tubes (stents) may be placed through the belly into the ureters to the kidneys. These help drain urine during healing.
-
If you have a neobladder, a catheter may be placed into it to help drain urine. If you have a pouch, a catheter may be placed through the stoma into the pouch. This is to keep the pathway open. Another catheter may be placed through the belly into the pouch. This is to help drain mucus and urine.
-
Once the surgery is done, the belly incision is closed with stitches or staples. A tube (drain) may be placed to drain excess fluid from the surgical area.
Recovering in the hospital
After the surgery, you will be taken to the post anesthesia care unit (PACU). There, you will be closely monitored as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain. Let your providers know if your pain is not controlled.
-
You’ll first have IV fluids only. In a day or so, you will start on a liquid diet. You will then slowly go back to a normal diet.
-
As soon as you’re able, you will get up and walk.
-
You’ll be taught coughing and breathing methods to help keep your lungs clear and prevent pneumonia.
-
A healthcare provider will show you how to care for your neobladder, or your pouch and stoma. You’ll also learn how to care for any drains and tubes that you have. You may be taught to flush your pouch with fluid to remove mucus.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your healthcare provider will tell you when you can go back to your normal routine. Until then, follow the instructions you have been given. Make sure to do the following:
-
Take all medicine as directed.
-
Care for your incision as instructed. If you go home with a drain or catheter, take care of them as you were shown.
-
If you have a stoma, care for it as instructed.
-
Follow your healthcare provider’s guidelines for showering. Don’t swim, bathe, use a hot tub, or do other things that will cover the incision with water. Wait until your provider says it’s OK.
-
Don't do any heavy lifting or strenuous activities as directed.
-
Don't drive until your provider says it’s OK. Don’t drive if you’re taking medicines that make you drowsy.
-
Walk a few times a day. As you feel able, slowly increase your pace and distance.
-
Don't strain to pass stool. If needed, take stool softeners as advised by your provider.
-
Do pelvic (Kegel) exercises as directed.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your provider
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worsening pain, or bad-smelling drainage
-
Pain, redness, swelling, odor, or drainage at the stoma site
-
Little or no urine output for longer than 4 hours
-
Burning or pain when passing urine or frequent need to pass urine
-
Bloody urine with clots
-
Leg pain or swelling
-
Problems with any drains, stents, or catheters
-
Nausea or vomiting that doesn’t go away
-
Pain that can't be controlled with medicine
Call 911
Call 911 right away if you have:
-
Chest pain
-
Trouble breathing
Follow-up care
You will have follow-up visits so your healthcare provider can check how well you’re healing. Stitches, staples, or tubes will be removed. You may be taught how to drain your pouch using a catheter. If you have a neobladder, you may be taught pelvic floor exercises to strengthen the muscles around it. This helps prevent urine leakage. You and your provider can also talk about any further treatment you may need.
Risks and possible complications
All procedures have some risk. Possible risks of this procedure include:
-
Bleeding (you may need a blood transfusion)
-
Infection
-
Blood clots
-
Pneumonia or other lung problems
-
Failure to remove all of the cancer, or cancer comes back
-
Problems with the neobladder or pouch
-
Development of stones in the neobladder or pouch
-
Problems with the stoma
-
Incontinence
-
Damage to the nerves that produce orgasm
-
Change to sexual satisfaction if a portion of the vagina is removed
-
Abnormal levels of vitamins and minerals in the blood, requiring lifelong medicine
-
Scarring and narrowing of the ureters
-
Bowel obstruction
-
Start of menopause
-
Risks of anesthesia (the anesthesiologist or nurse anesthetist will discuss these with you)